Hemi-Laryngopharyngeal Spasm (HELPS syndrome)
Our sentinel paper describing the world’s first recognized case of HEmi-LaryngoPharyngeal Spasm or HELPS was published in the Journal of Neurosurgery (in July 2016).
.
Here is a link to the paper.
.
Our more extensive description of three additional cases of HELPS was published in the Journal of Neurosurgery (in July 2018).
.
Here is a link to the paper.
.
Our paper describing the MRI findings in HELPS was published in the American Journal of Neuroradiology (in Oct 2018).
.
Here is a link to the paper.
.
Our paper demonstrating the connection between glossopharyngeal neuralgia and HELPS was published in Neurosurgery (in December 2019). It also discovered 27 previous descriptions of patients with HELPS, unrecognized at the time, from six different countries in four different languages.
.
Here is a link to the paper.
.
Dr. Amanda Hu, in collaboration with Professor Murray Morrison, has published a paper reviewing the diagnosis of HELPS for otolaryngologists. This was published in 2020 in the Annals of Otology, Rhinology, & Laryngology.
Here is a link to the paper.
.
.ff
HELPS syndrome
HELPS syndrome is a condition caused by a blood vessel pinching the nerve rootlets of the Vagus nerve (the Xth cranial nerve). It is similar to the well recognized hemifacial spasm syndrome but the nerve involved is the Vagus instead of the Facial nerve. As a result, the symptoms are episodic throat contractions and cough. The throat contractions typically become stronger and more frequent over the years and can lead to a terrifying inability to breath or choking sensation. Patients may end up in the Emergency Department being intubated or with a permanent tracheostomy because of their inability to breath during a severe episode. Some but not all of our patients can tell which side of their throat (left or right) contracts during a choking episode. In between these choking episodes, patients feel normal.
Physicians unfamiliar with this condition may misdiagnose HELPS syndrome as a psychiatric conversion disorder, a response to gastric reflux, or laryngeal dystonia. One identifying feature is that the spasms eventually occur while sleeping. Another feature of this condition is that it is associated with coughing episodes. These coughing spells usually begin as a response to a tickling sensation at the back of the throat. In response to this tickling sensation, the patient will cough. This coughing tends to get stronger over the years and eventually can be so severe that it causes dizziness (“seeing stars”), vomiting or urinary incontinence. Our patients have described various triggers for this coughing including environmental odors, prolonged or loud talking but it can also occur spontaneously without any obvious cause. Eventually the coughing will occur while sleeping.
Diagnosis
The diagnosis of HELPS syndrome requires a history of intermittent choking and coughing. We have published our guidelines for the diagnosis of this condition (see above paper). Obvious causes need to be excluded including acid reflux, exposure to airborn irritants, conversion disorder and dystonia. Laryngoscopy can sometimes see a unilateral twitch of a vocal fold following vocalization. This is pathognomonic and not seen in any other condition. The choking will be reduced by unilateral botulinum toxin (Botox) injections on the side of the problem but will have no effect on the opposite side. These tests should be spaced in time to give the vocal fold time to recover completely from the first injection before trying the second side. If there is a unilateral response to the Botox injections and an MRI demonstrates a vessel encroaching on the vagus nerve on the same side, then neurosurgery can be discussed.
Treatment
Patients can be treated with repeated Botox injections. The throat spasms will still occur but will be much less severe. These injections typically need to be repeated every three months. This will not stop the coughing because the tickling sensation continues. The coughing may respond to anti-neuralgia medications such as carbamazepine or amitriptyline. If patients want an opportunity for a definitive cure, then the pinched vagus nerve must be decompressed surgically. This operation is called a microvascular decompression (MVD). Many neurosurgeons will be familiar with the MVD operation for trigeminal neuralgia (Vth cranial nerve), hemifacial spasm (VIIth cranial nerve), or glossopharyngeal neuralgia (IXth cranial nerve). The operation is essentially the same except the nerve being decompressed is the Vagus (Xth cranial nerve).
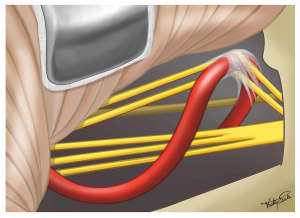
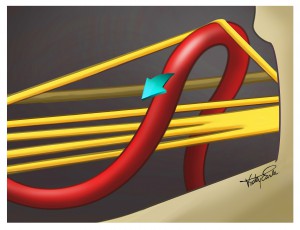
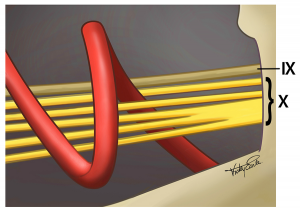
During the world’s first successful operation to cure this condition, we saw that two of the rootlets forming the patient’s Vagus nerve were severely stretched by a loop of the posterior inferior cerebellar artery (see Figure 1 below). After we freed the rootlets from some scar tissue, one of them fell back into the normal position (see Figure 2 below). We then moved the artery slightly to free up the second rootlet (see Figure 3 below). The patient did well with no surgical complications and has not had another episode of HELPS in over 4 years.
Figure 1:
The top two of the five rootlets making up the Vagus nerve (cranial nerve X) in this patient were obviously distorted by the posterior inferior cerebellar artery. The glossopharyngeal nerve (cranial nerve IX) was not affected.
Figure 2:
After freeing up some scar tissue around the rootlets, one of them fell back into the normal position. We then moved the artery slightly to take the pressure off the other affected rootlet.
Figure 3:
At the conclusion of the operation, all the nerve rootlets were safely decompressed.
Listen to a patient describe their symptoms
We are very grateful to our patients for sharing their stories. In the video below, “Patient #2” describes his HELPS syndrome before and 8 months after MVD surgery.
.
Future Work
First, we are working to clarify the diagnosis of this condition. It is likely that patients will present with slight variations of symptoms and we want to understand what are the common themes (e.g. throat contractions and cough) and what are the less commonly associated problems (e.g. changes in voice or a feeling of a fat tongue). We also want to understand what is the best method of conclusively diagnosing this condition. We believe that the unilateral vocal fold twitch described in our paper is unique to this condition. Not all patients will have this (or it will not be present during the examination). A unilateral improvement in throat contractions following Botox with no improvement on the other side is suggestive of a unilateral problem. If the MRI shows a vessel encroaching on the vagus nerve on the same side then that is highly suggestive of HELPS on that side.
Second, we are working to educate our colleagues around the world that HELPS exists and can be cured. This will be done with publication of our work in peer-reviewed journals and presentations at scientific conferences. Our peer-reviewed papers (see above) are available for our colleagues to read and learn about HELPS syndrome. We have presented our first case to our North American neurosurgical colleagues at the American Society for Stereotactic and Functional Neurosurgery (ASSFN) in June 2016 and presented our first four cases to our European colleagues at the European Society for Stereotactic and Functional Neurosurgery (ESSFN) meeting in September 2016. Our first five cases were presented to the World Society for Stereotactic and Functional Neurosurgery (WSSFN) at their quadrennial meeting in Berlin June 2017 (on the last lecture of the final day of the meeting!). Dr. Honey has also presented this work as an invited guest at the 4th annual Russian Federation of Stereotactic & Functional Neurosurgery meeting in Moscow (May 2018) and as a guest of the Iranian Neurosurgical Society (May 2018).
Third, although the surgical cure will lie in the hands of neurosurgeons, the diagnosis (and thus access to care) will depend on our ENT and Emergency Medicine colleagues. We will have to educate them as well about HELPS. It is unfortunate that all our patients were told at one time during their illness that they had a psychiatric illness. This is a misdiagnosis but a common medical error when the physician does not recognize the illness. The stress of being misdiagnosed can lead to anxiety for our patients. They tend to avoid any food or activity that happened to precede their last severe episode and therefore they can develop some obsessive-compulsive traits. Finally, being told “it’s all in your head” can make some patients angry. The combination of anxiety, obsessive-compulsive traits and anger can mislead a psychiatrist into believing that the patient does have a psychiatric disorder. VANCOUVER syndrome is a physical illness and it has a surgical cure.
Ultimately, we need other centers to be able to recognize and treat this condition.
The picture below is a close-up of a self portrait by Frieda Kahlo entitled “Self portrait with thorn necklace and hummingbird” (Autorretrato con collar de espinas y colibrí ) from 1940. The constricting necklace reminds me of the throat contractions of hemi-laryngopharyngeal spasm.