Dental Neuralgia or Anesthesia Dolorosa
This information is designed to help patients talk to their neurosurgeons about their facial pain. It is not intended to give specific treatment guidelines.
Introduction
There are two different types of physical pain: nociceptive and neuropathic. Nociceptive pain is the body’s normal response to a painful stimulus. This pain is crucial for survival and strongly linked with learning. When you touch a flame it hurts and you learn quickly not to do that again. Neuropathic pain is an abnormal pain that occurs after damage to the pain pathways (nerves, spinal cord or brain). It should never happen and serves no purpose. It is the brain’s misinterpretation of signals coming from a damaged nerve pathway. The classic example is phantom limb pain. This was first described in the American civil war when soldiers survived an injury where they lost a limb – and they could still feel pain in that missing limb.
There are many different pathologies that can cause pain in the face. The most common causes are dental (e.g. sore tooth) and sinus pain (e.g. sinusitis). Our clinic has focused on the types of pains caused by neurological conditions. These include the following:
trigeminal neuralgia
post-herpetic neuralgia
de-afferentation neuropathic facial pain
dental neuralgia (nerve damage pain following a dental procedure)
Before you can begin treating a medical problem, you must understand its cause. This is true regardless of the medical condition but is absolutely crucial when dealing with facial pain. The perfect operation for trigeminal neuralgia will not help post-herpetic neuralgia. It is therefore vitally important that the first step in treating a facial pain condition is making the correct diagnosis. The famous French neurologist, Jean-Martin Charcot (1825-1893), said “To learn how to treat a disease, one must learn how to recognize it. The diagnosis is the best trump in the scheme of treatment.”
De-afferentation Neuropathic Facial Pain
There are many different names for this pain syndrome and there are some subtle differences that are important. ‘Dental neuralgia’ describes the neuropathic pain following injury to a nerve to a tooth – usually caused by a dental procedure. ‘Anesthesia dolorosa’ describes the neuyropathic apin following injury to the trigeminal nerve to the face – usually caused by a surgical procedure (e.g. rhizotomy). The conditions all have the same cause – a nerve injury causing a ‘central pain syndrome’. Patients who have a stroke causing numbness in their face will also sometimes get a very similar pain syndrome – ‘post-stroke facial pain’.
The best analogy to understand this phenomenon is phantom limb pain. Patients who have lost a limb occasional develop a pain syndrome in the absent limb. They may have no leg but their missing foot hurts constantly. This is due to the abnormal changes in the brain dealing with the leg region. Even though there are no signals of pain coming from the foot (because it is not there) the region of the brain that would be activated by pain signals coming from the foot is somehow spontaneously active. This produces a constant pain that can be describes as burning, twisting, crushing, or a bursting pressure. Usually the pain varies throughout the day (usually getting worse as the day progresses) but it is often described as reaching a “10 out of 10” and it never goes away.
The same phenomenon can happen in the face or teeth if a branch of the trigeminal nerve is injured or completely cut. The most frequent cause of this is a dental surgery mistake. If one of the nerves to the teeth is damaged during a dental procedure, the area it was innervating will be immediately numb. Later (sometimes up to a year later) the numbness turns into a burning discomfort that heralds the onset of neuropathic pain. In this scenario, it is very common for the dentist to try additional procedures, incorrectly assuming the original cause for the pain has not been cured. In fact, this is a completely new type of pain – a neuropathic pain.
De-afferentation neuropathic facial pain can be caused anytime the normal sensation from the face is damaged. This can be from a peripheral cause such as cutting a branch of the trigeminal nerve (during a dental surgery or following a skull fracture when the nerve is cut by the fractured edge of the skull) or from a central cause (when the facial sensation pathway is destroyed by a stroke).
The treatment of this condition will require a pain specialist with experience in this area. The great variety of medications recommended for this condition suggests that no one medication is clearly effective. Often a combination of powerful medications is required (including antidepressants and antiepileptics) to numb the pain. The continuous stress of this chronic pain often leads to depression and can destroy the patient’s family relationships.
If all medications fail, patients may benefit form surgical intervention. Facial (not tooth) neuropathic pain can respond to an operation called Motor Cortex Stimulation. Up to 70% of patients get more than half their pain reduced. Neuropathic pain in the teeth may respond to thalamic deep brain stimulation.
The Surgical Treatment of Facial De-afferentation Pain
Motor Cortex Stimulation
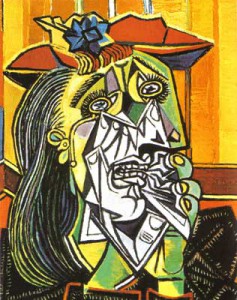
The picture below is of Picasso’s “Weeping Woman” from 1937. The disfigured face and suffering represents the disorder nervous system and resulting pain following dental nerve injury.